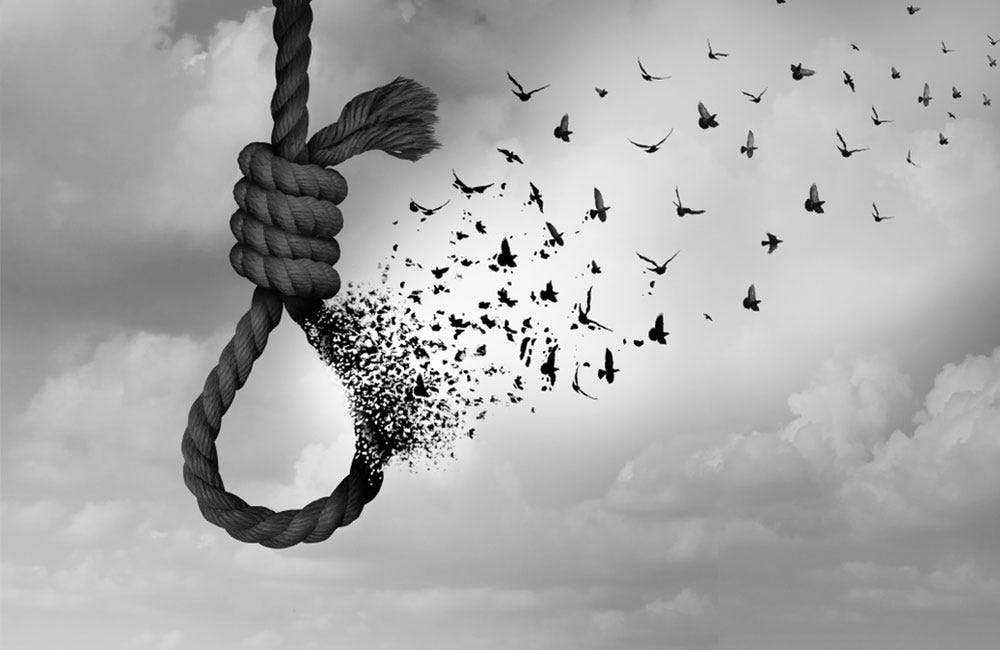
When Suicide Feels Like the Only Way Out..
The hidden reason so many never seek help...
and what we can do about it?
Thousands of people die by suicide each year without ever seeking help beforehand. Even in countries with excellent mental health services and strong prevention efforts, like Denmark, more than half of those who die by suicide never make contact with a professional.
This is partly due to external barriers like stigma, fear of not being understood, and the dread of forced hospitalization. But there are also deep, internal reasons. In a survey of 8,400 individuals who had experienced suicidal thoughts in the past year, three-fourths felt they didn’t need mental health treatment. In another study, over half of people who had attempted suicide believed no one could have prevented it, and only a small percentage mentioned a health professional.
Why does this happen?
How Suicide Can Feel Like a “Logical” Goal
In psychological terms, "ego-syntonic" describes thoughts or behaviors that feel in line with a person's identity. For many in crisis, suicide becomes ego-syntonic seen as normal or even necessary. When someone feels deeply worthless or broken, ending their life can appear to be the most rational solution to escape unbearable pain.
Emotional distress and tunnel vision can push someone into this mindset, making suicide seem not only acceptable but inevitable. Interestingly, after a suicide attempt, many people experience a sudden shift. Survivors often describe an immediate realization of regret the moment they act—what’s known as switching from ego-syntonic to ego-dystonic thinking.
This switch shows that suicidal thinking can be like a mental “mode” that turns on and off. It also explains why our usual protective “system 2” thinking slow, conscious, rational fails to override impulsive, automatic “system 1” decisions in these moments.
A New Approach: Seeing and Confronting One's Own Story
ASSIP (Attempted Suicide Short Intervention Program) is a person-centered, three-session therapy designed for people after a suicide attempt. In the first session, patients tell their story on video. In the second, they watch this video with their therapist, stepping into an observer’s role.
This process helps patients confront their own narrative and understand how suicide became a perceived solution. With guidance, they learn to identify triggers and warning signs and develop safety plans.
In a study with 120 patients, ASSIP reduced the risk of future attempts by 80% over two years. One patient described feeling "unburdened" after this process, noting that watching the video made it clear how “silly” and tragic the idea of suicide really was.
Rethinking the Traditional Medical Model
The traditional medical approach treats suicide as an illness, expecting that people in crisis will seek help. But many don’t, because their suicidal thoughts feel deeply personal and in line with their current sense of self.
A purely illness-focused model often misses "the person in the patient." People need to understand their own dynamics, vulnerabilities, and triggers to prevent future crises.
Moving Toward Person-Centered Care
We must go beyond viewing suicide only as a risk to be managed. Therapists and health professionals need to build collaborative relationships with patients, working together to understand each person’s unique experiences and psychological pain.
A person-centered approach, where patients and professionals explore individual stories and vulnerabilities together, can be more effective in preventing suicide than focusing solely on risk factors.
Summary
Thousands die by suicide without ever reaching out for help. One crucial, often overlooked reason is that suicide can feel like an ego-syntonic goal—consistent with one’s sense of self. Understanding and addressing this psychological experience through personal, collaborative approaches can help bridge the gap between those in crisis and the support they need.





One of the most troubling aspects of today's world is how increasingly isolated people are becoming.
The worst part is knowing that the people who know this still won’t do anything about it. And the ones willing to do something don’t really know what to do or how to empathize in an effective way, because they are intimidated.